
Fractured Teeth
Fractured teeth are usually caused by either trauma to the head and mouth or from pets chewing on hard objects such as bones. Often fractured teeth go unnoticed by the owners unless they observe the injury causing the fracture. Veterinarians and technicians often find fractured teeth when performing oral examinations and dental treatment.
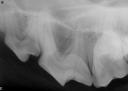
In order to determine the best treatment for fractured teeth, physical and radiographic evaluations are essential. Limited physical examinations can be done in the exam room while more thorough evaluations must be performed while the patient is anesthetized.
Once the patient is anesthetized, physical evaluation can be performed on the fractured teeth using a dental explorer, transillumination (directing a small concentrated light source on a tooth), and a periodontal probe.
A fine pointed dental explorer is used to probe the dental tissues for loose fragments, cracks, multiple fracture planes, dentin / enamel separation, exposed pulp chambers or pulp canals. A periodontal probe is used for exploring the extent of slab fractures that extend below the gumline. Transillumination can help reveal vertical fractures as well as determine tooth vitality. A vital tooth will have a translucent appearance while a non-vital tooth will appear opaque.
In order to complete the evaluation process, dental radiographs of the fractured tooth as well as the contra-lateral tooth should be taken.
A simple crown fracture involving only the enamel may only require smoothing the enamel (odontoplasty) with a fine diamond bur in a water-cooled high-speed hand piece as long as there is no radiographical evidence of abscess.
Crown fractures involving enamel and dentin without pulp exposure may also be restored using dental adhesives or sealants, and composites after taking a dental radiograph to rule out signs of pathology. After the radiograph is assessed, the tooth can be smoothed and the enamel beveled. The fractured tooth is then cleaned, polished with flour of pumice, etched and treated with a dental adhesive or sealant. A composite filling material can then be placed over the fracture to restore the tooth.
If the fractured tooth has signs of a near pulp exposure (pink spot in the dentin over the area of the pulp chamber), a dental radiograph should first be taken to evaluate the fractured tooth for signs of pathology. If there are no signs of pathology then the near pulp exposure should be treated prior to restoring the tooth. Restoration would be performed as previously described.
If the vital pulp is exposed, performing a partial pulpectomy and medicating the pulp (pulp capping) may be an option provided radiographs of the tooth are normal. It is recommended that a partial pulpectomy and pulp cap be performed only in recent tooth fractures (24-48 hours since exposure in a mature dog, or up to 2 weeks exposure in a dog less than 18 months of age). After performing a partial pulpectomy and pulp cap, the tooth is restored with adhesives and composites as described above. If the fractured tooth with pulp exposure does not meet the criteria for partial pulpectomy and pulp capping then root canal therapy is indicated before restoring the fractured tooth.
A fractured tooth with a non-vital pulp usually presents as a crown or crown-root fracture and black (necrotic) pulp. This type of fracture can be treated with root canal therapy followed by restorative treatment with adhesives and composites or metal crowns.
It takes 6 -12 months for pathological signs of disease to appear on a dental radiograph, therefore follow-up dental radiographs should be taken of any fractured tooth 6-12 months after treatment to ensure the pulp is healthy and there are no signs of pathology.If a client declines treatment of a fractured tooth with pulp exposure, then an extraction should be recommended. Leaving a tooth with pulp exposure untreated is not an option because it can result in an unnecessary and painful infection for the patient.








You must be logged in to post a comment.